What Is Assisted Living?

Find assisted living near you
There are different types of long-term residential facilities available to seniors, and each accommodates residents with varying needs. While seniors living in independent living facilities need little to no help with daily activities, those in nursing homes or memory care facilities may require around-the-clock assistance and skilled medical services. Assisted living facilities, or ALFs, are intended for seniors whose needs fall somewhere in between.
Assisted living staff help residents with some (but generally not all) activities of daily living (ADLs), such as bathing, dressing, and eating. ALFs also help with errands such as housekeeping and transportation. They do not typically offer regular skilled nursing services, though emergency help is always available.
For support in determining if assisted living is the right fit for your loved one and what facility might be their best option, reach out to Caring.com’s Family Advisors at (800) 558-0653. These friendly experts can simplify the decision-making process, and their services are free of charge.
Key Takeaways
|
How To Know When It's Time For Assisted Living
It may be time to move to an assisted living facility when performing ADLs becomes difficult or impossible. When you or your senior loved one can no longer perform routine activities, it can negatively affect you or your loved one’s well being. Continuing to live independently may become unsafe.
Indications assisted living services may be needed include:
- Sudden or increasing weight loss or frailty
- Declining personal hygiene, including soiled clothing or unkempt hair
- Accidents or injuries occurring in or outside the home
- Signs of loneliness, isolation, or depression due to lack of companionship
- Unpaid bills and loans or unopened mail from creditors
- Stale or spoiled foods and beverages in the pantry and refrigerator
- Broken and unrepaired appliances that were once used regularly
- An increasingly disorganized or unclean home
| Continue Reading: How to Know When It's Time for Assisted Living |
Is Assisted Living Right for You?
If you are in good overall health and can perform everyday tasks on your own, you may enjoy residing in an independent living facility. These facilities typically provide food, entertainment, socializing opportunities, housekeeping, and more, but don’t generally offer assistance with personal care or skilled medical services.
However, if you or your loved one can no longer function well independently and need help with ADLs, assisted living facility services can give you the additional support you require.
It is also important to recognize if your needs are greater than those that can be accommodated at home with in-home care or at assisted living communities. If you need assistance with most or all daily tasks, require ongoing skilled medical care, and/or have memory impairment, a nursing home or memory care facility might be a better fit.
Assisted Living vs. Other Types of Senior Care
If you’re unsure if assisted living is right for you, one of the other types of senior care may be a better fit. See how they compare below.
| Care Type | Shared Spaces + Group Activities | Offers housekeeping | Offers Assistance with ADLs* | Offers skilled nursing services | Assistance available 24/7 |
|---|---|---|---|---|---|
| Assisted Living | ✔ | ✔ | ✔ | ✔** | ✔ |
| In-Home Care | ✗ | ✔ | ✔ | ✗ | ✗ |
| Home Health Care | ✗ | ✔ | ✔ | ✔ | ✗ |
| 55+ Communities | ✔ | ✗ | ✗ | ✗ | ✗ |
| Independent Living | ✔ | ✔ | ✗ | ✗ | ✗ |
| Memory Care | ✔ | ✔ | ✔ | ✔** | ✔ |
| Skilled Nursing Homes | ✔ | ✔ | ✔ | ✔ | ✔ |
| Continuing Care Retirement Communities | ✔ | ✔ | ✔ | ✔ | ✔ |
*Activities of Daily Living. Learn More About ADLs.
**Regular skilled nursing care is sometimes, but not always, offered in assisted living and memory care communities.
Learn how assisted living compares to other types of senior care
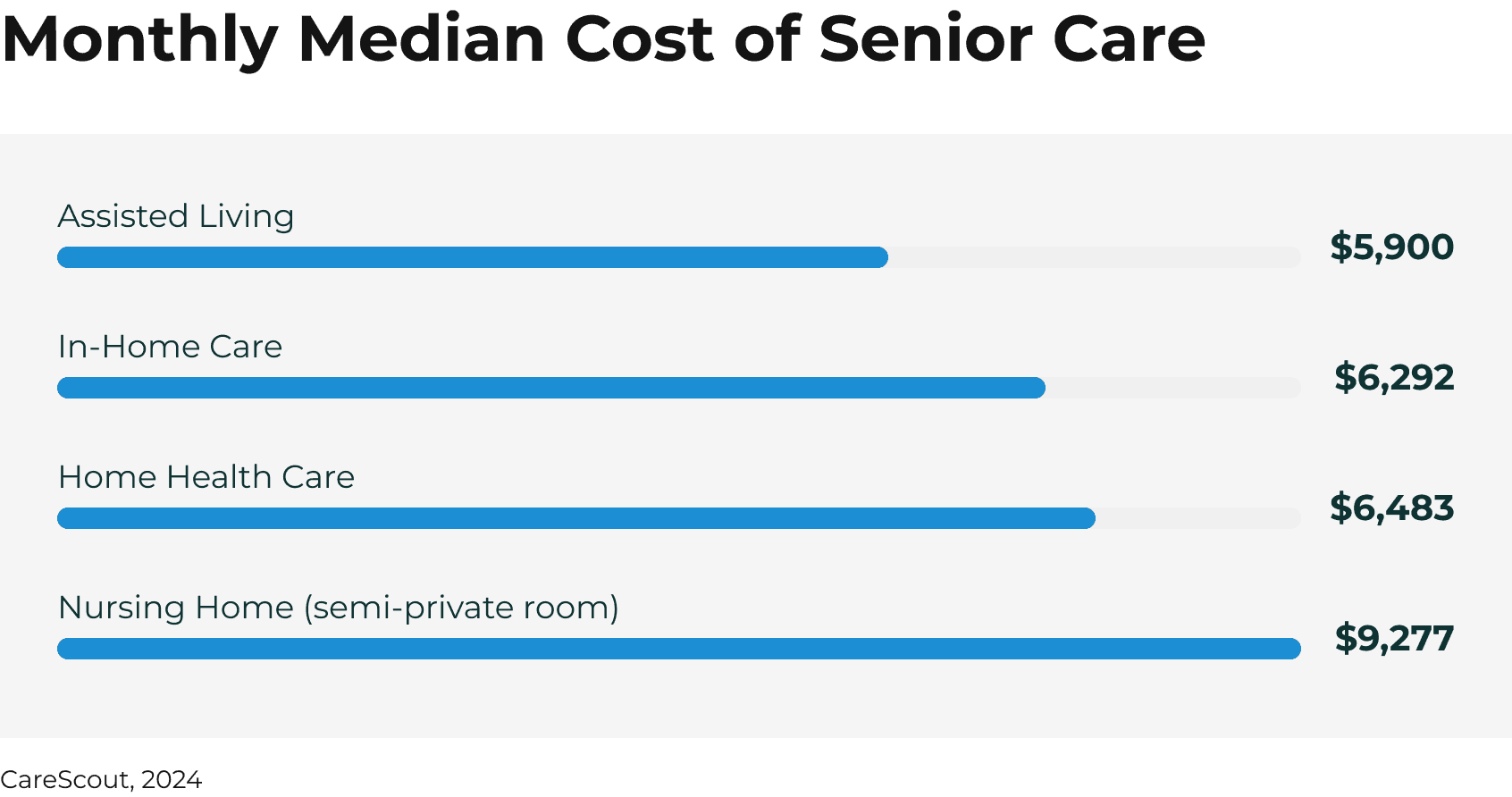
How Much Does Assisted Living Cost?
As of 2023, the national median cost of assisted living for seniors is $5,350 per month. This can vary drastically depending on several factors including location and type of community:
- Location: Costs vary significantly in different areas of the country. If you live in a high-cost-of-living area, expect to pay on the high end for assisted living. However, remote areas where assisted living isn’t widely available may also be expensive due to scarcity.
- Type of Community: While all assisted living communities provide assistance with ADLs, the “extras” can vary significantly. Luxury assisted living communities will have upgraded amenities and services like on-demand concierge or on-site golf courses, while less expensive facilities will have fewer lifestyle services and may have older construction.
- Individual Services Needed: Some communities have additional fees for services that go beyond help with ADLs, such as physical and occupational therapy.
- Cost Structure: Some ALFs charge an all-inclusive monthly fee, while others may charge for specific items or services like therapy, group outings, or food, drinks or snacks eaten outside of mealtimes.
How to Pay for Assisted Living
Assisted living communities are not medical facilities, and are therefore not covered by Medicare. Similarly, standard Medicaid does not include assisted living among its covered services.
However, many states offer Medicaid waivers, add-ons to standard Medicaid, that can help seniors pay for assisted living. Additional options that can make assisted living more affordable, include:
- Veteran benefits: The VA covers long-term care services for qualifying sick or disabled veterans in assisted living centers as well as in-home or at other types of facilities.
- Long-term care insurance: Policy terms and coverage vary, but many long-term care insurance plans with assisted living coverage reimburse out-of-pocket costs up to a set annual amount. However, LTC insurance is harder to get approved for if you wait until you need it; your current health status impacts whether or not you get approved for an LTC policy.
- Annuities: Immediate or deferred long-term care annuities purchased through an insurance company provide regular payments that can be used for assisted living costs.
- Reverse mortgages: Reverse mortgages convert home equity into non-taxable income that can help pay for assisted living.
- Life insurance payouts: Cash out your life insurance policy, purchase a policy with combined long-term care benefits, or use accelerated death benefits to cover assisted living costs.
Learn more about these and other available options that may be available to you or your loved one and help cover the costs of assisted living.
Top resources for seniors and caregivers
Assisted Living FAQ
Browse our answers hub to find all the answers to your senior care questions.
How to Find Assisted Living
Caring.com’s expert Family Advisors provide no-cost, personalized advice and recommendations for care seekers like you. Call (800) 558-0653 to speak with an advisor and start the process of finding the right assisted living community for you.
Top Assisted Living Locations
View assisted living options in the top-searched locations.
Don't see your location? Find assisted living near you.
Select your state and browse our filterable database to begin
- Alabama
- Alaska
- Arizona
- Arkansas
- California
- Colorado
- Connecticut
- Delaware
- District Of Columbia
- Florida
- Georgia
- Hawaii
- Idaho
- Illinois
- Indiana
- Iowa
- Kansas
- Kentucky
- Louisiana
- Maine
- Maryland
- Massachusetts
- Michigan
- Minnesota
- Mississippi
- Missouri
- Montana
- Nebraska
- Nevada
- New Hampshire
- New Jersey
- New Mexico
- New York
- North Carolina
- North Dakota
- Ohio
- Oklahoma
- Oregon
- Pennsylvania
- Rhode Island
- South Carolina
- South Dakota
- Tennessee
- Texas
- Utah
- Vermont
- Virginia
- Washington
- West Virginia
- Wisconsin
- Wyoming











